Page 18 - Science Focus (Issue 018)
P. 18
“Assembling” Our Weapon From Scratch
So, how do we actually create CAR-T cells? Once
the desired protein domains have been chosen, we
will fuse their respective DNA sequences together and
integrate them into the genome of a T cell sourced from
the patient’s own body by some genetic engineering
techniques in a lab. This brings CAR-T cells into existence
because the cells will now be able to produce the
customized weapon (the said chimeric receptor) with
our lines of commands (the DNA sequences). The CAR-T
cells are re-delivered back into the patients’ body
afterwards as a “living drug”.
Efficacy and Challenges
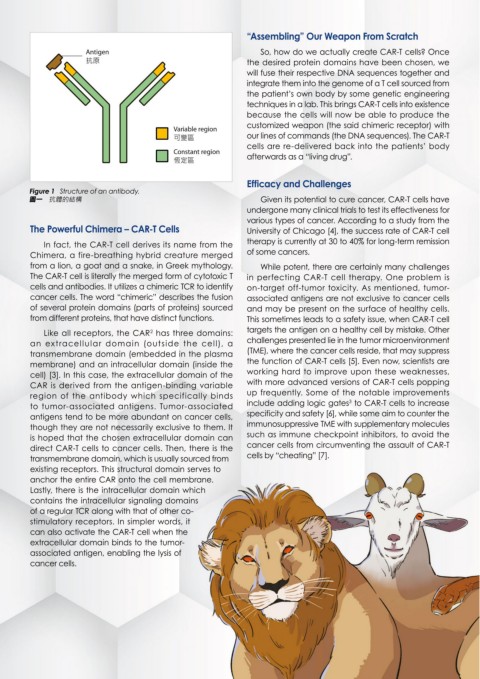
Figure 1 Structure of an antibody.
ྡɓ 抗體的結構 Given its potential to cure cancer, CAR-T cells have
undergone many clinical trials to test its effectiveness for
various types of cancer. According to a study from the
The Powerful Chimera – CAR-T Cells University of Chicago [4], the success rate of CAR-T cell
In fact, the CAR-T cell derives its name from the therapy is currently at 30 to 40% for long-term remission
Chimera, a fire-breathing hybrid creature merged of some cancers.
from a lion, a goat and a snake, in Greek mythology. While potent, there are certainly many challenges
The CAR-T cell is literally the merged form of cytotoxic T in perfecting CAR-T cell therapy. One problem is
cells and antibodies. It utilizes a chimeric TCR to identify on-target off-tumor toxicity. As mentioned, tumor-
cancer cells. The word “chimeric” describes the fusion associated antigens are not exclusive to cancer cells
of several protein domains (parts of proteins) sourced and may be present on the surface of healthy cells.
from different proteins, that have distinct functions. This sometimes leads to a safety issue, when CAR-T cell
Like all receptors, the CAR has three domains: targets the antigen on a healthy cell by mistake. Other
2
an extracellular domain (outside the cell), a challenges presented lie in the tumor microenvironment
transmembrane domain (embedded in the plasma (TME), where the cancer cells reside, that may suppress
membrane) and an intracellular domain (inside the the function of CAR-T cells [5]. Even now, scientists are
cell) [3]. In this case, the extracellular domain of the working hard to improve upon these weaknesses,
CAR is derived from the antigen-binding variable with more advanced versions of CAR-T cells popping
region of the antibody which specifically binds up frequently. Some of the notable improvements
3
to tumor-associated antigens. Tumor-associated include adding logic gates to CAR-T cells to increase
antigens tend to be more abundant on cancer cells, specificity and safety [6], while some aim to counter the
though they are not necessarily exclusive to them. It immunosuppressive TME with supplementary molecules
is hoped that the chosen extracellular domain can such as immune checkpoint inhibitors, to avoid the
direct CAR-T cells to cancer cells. Then, there is the cancer cells from circumventing the assault of CAR-T
transmembrane domain, which is usually sourced from cells by “cheating” [7].
existing receptors. This structural domain serves to
anchor the entire CAR onto the cell membrane.
Lastly, there is the intracellular domain which
contains the intracellular signaling domains
of a regular TCR along with that of other co-
stimulatory receptors. In simpler words, it
can also activate the CAR-T cell when the
extracellular domain binds to the tumor-
associated antigen, enabling the lysis of
cancer cells.